Welcome to Meet a Library User. This blog series highlights some of the many MSK employees who use the Library and the fascinating work that they accomplish.

In this post, we’re speaking with Dr. Lisa Diamond, MD, MPH. Dr. Diamond is a member of the research faculty in the Immigrant Health and Cancer Disparities Service, a part of the Department of Psychiatry and Behavioral Sciences. Her clinical work is as an MSK hospitalist under the Department of Medicine in the Hospital Medicine Service. It is a pleasure to speak with Dr. Diamond and learn about her research and its impact at MSK.
The following conversation has been edited and condensed.
Could you discuss, in simple terms, your research agenda and a project that you’re working on now?
My research is on language barriers and how they affect quality of care and outcomes, particularly in cancer, but it’s obviously a health equity issue that crosses multiple disease states and health situations, so it extends beyond cancer. I’m particularly interested in language concordance and how when physicians and nurses speak a patient’s language, how that affects their quality of care.
I’ve looked at this in a number of ways and often look at physician behavior with using their language skills—the ultimate question being how fluent is fluent enough to use your language skills? Some of the research I’ve done has looked at this issue and has led to policy change, including here at MSK. We’re going to be implementing a bilingual proficiency program, based on evidence from the literature that I published, that helps gauge somebody’s language proficiency level and whether they are at the point where they’re ready to be using those skills with patients directly.
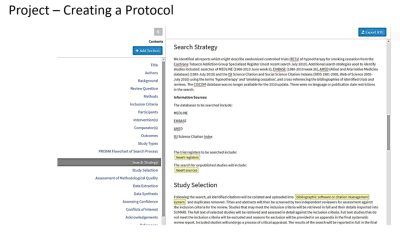
As for a project right now, I have a systematic review that I’m working on with some students and a predoc that’s looking at patient satisfaction in cancer care by race, ethnicity, and language. There’s a lot of lore in the health system world—where we value patient satisfaction data greatly. There’s all this lore about different groups and how they report on the quality or their satisfaction with the care that they’ve received. The lore being that Chinese speakers are less satisfied overall with their care and Hispanics are often very satisfied with their care. And I wanted to know if this lore was true by looking at a synthesis of the literature. So we looked at any paper looking at patient satisfaction and cancer.
Some of the papers are revealing that the lore has cultural implications. So maybe people are overly reporting satisfaction because culturally they would never say anything negative about a physician. Or on the opposite side, maybe the way we’ve translated the materials makes people report seemingly lower satisfaction, but they’re not actually unsatisfied, it’s just the way we ask the question and the way we translated the question. So it may have less to do with lower satisfaction and more to do with asking the wrong questions to people who don’t speak English. It’s really interesting, and we’re working on synthesizing that and publishing hopefully by the end of the year.
It’s informative to look back at previously published studies and see them in a new light that way. Could you talk about how you first became interested in health disparities among immigrant populations and non-English-language speakers?
I am a second-language-learner of Spanish. I would say I’m proficient enough to use my skills in patient care, and I’ve had testing to show that, but I’m not a native speaker. I noticed in medical school and residency that I had certain thresholds at which I would say, even though I speak Spanish comfortably, I really need to get an interpreter here. One example of that is goals of care discussions. Whenever I was talking to a patient about whether they wanted to be DNR [do-not-resuscitate] or we were going to shift goals of care, I realized that these are challenging conversations to have in English, and if I tried to then say it in Spanish, even though I could, I was worried about my word choice. I felt concerned knowing these are conversations that patients and family members remember forever, right? You hear that from families, that they remember. If I’m the person telling someone they may not survive, and we need to talk about it—the words I use are words that stay with that family forever. The nuance of language is always important, but particularly important in those sensitive and emotional situations.
I started to think, is there a threshold above which I would feel comfortable doing this or will I always feel uncomfortable doing this because I’m not a native speaker? And is that OK? I mean, is this a black and white thing? Where if I’m good enough to use my Spanish skills, I should always use them? Understanding the nuances of that spectrum was really important and interesting to me. And that’s what led to the research, let alone seeing a lot of people do what I call ‘getting by,’ which is when someone might speak a little Spanish and they’ll use it in clinical care. And it can be to the detriment of the patient care experience. I would see colleagues doing this in residency. It happens a lot where people sort of wing it, and it’s not adequate communication, particularly when you recognize that a large percentage of our diagnostic work-up comes from taking a good history and doing a good physical exam. And if you can’t do either of those things because you’re not really communicating effectively with the patient, that’s a problem. So that’s where the interest started.
What are some steps that current and future health care professionals can take now to better serve diverse populations?
I think one of the most important things is recognizing one’s own limitations in a language. If you do speak another language, no one is saying you can’t chat, greeting a patient in their primary language and building rapport is wonderful, but when it comes to talking about medical decision making or instructions or anything beyond your linguistic abilities, recognizing that those abilities are limited and getting the interpreter in to help you. I think their goal is to make sure that the communication is effective, so partnering with the interpreter to do that and maybe even having a conversation before the patient is physically in the room to say, ‘this is what I hope to get from this conversation’ so that you can set goals and have them be a part of the health care team as they should be. That’s what I would consider.
In addition to being an MD, you have a master’s in public health. Has living through the COVID-19 pandemic changed how you think about public health issues?
Yeah, there’s so much to that question. I think between being a physician during COVID, being trained in public health, and being a parent of kids in the school system during COVID, it was a fascinating lesson in the power and the weakness of population-based data to make decisions for individuals.
One of the things that we are unfortunately lacking greatly is communication, effective communication strategies between scientists and the public. That was particularly stark when it came to language barriers. Our messaging to communities who didn’t speak English was really lacking, and there’s a lot of misinformation going around, which led to further disparities that were already present when the pandemic hit. So effective communication strategy is a huge need and something that public health absolutely needs to focus on.
Final question, would you share some of the ways that you use MSK library?
Oh gosh, I constantly use the MSK library. I mean, the journals that I need to access aren’t always cancer journals, and they may not be indexed journals, so I’m regularly asking for outside articles [via Document Delivery Services]. That’s a very common, probably weekly occurrence for me. Especially because my work is cross disciplinary, I end up needing articles in all kinds of areas. I’ve lost track of how many systematic reviews I’ve done, but I’m regularly working with the library on systematic reviews. And I always send students and residents and fellows – everyone – I regularly send them to the Library for classes and one-on-one coaching with librarians. The research informationists are amazing and supportive and generous with their time.
I’ve never worked at an institution that was so well-supported by a library as this one. I brag about it all the time because my colleagues don’t have this. They may have a research librarian they can go to and ask questions, but as a team, this library is really unparalleled. And I’m not just saying that because we’re in an interview, but it is pretty remarkable what this library does to support faculty.
Many thanks to Dr. Diamond for speaking with us. If you would like to know more about MSK Library’s services, please see our Help page. And if you already use the Library and would like to be featured in this series, don’t hesitate to reach out!
Interview by Rebecca Meng, MSLIS